Saturday 07 March, 2026
|
نبذة عن المجلس العلمي لجراحة الأنف و الإذن و الحنجرة |
تأسس المجلس العلمي لجراحة الأنف و الإذن و الحنجرة سنة 1988 و مدة الدراسة فيه خمس سنوات حيث يهدف المجلس إلى تطوير المهارات العلمية والعملية والتطبيقية لطلبة مجلسنا العلمي والعمل على إجراء دورات مستمرة لتحديث المعلومات وكسب المهارات وفق التقنيات الحديثة للرقي إلى مستوى يضاهي التقدم الحاصل في الجامعات العالمية ويلبي متطلبات المجلس العراقي للاختصاصات الطبية
اللجنة المؤسسة : أعضاء المجلس العلمي هم :
1-الأستاذ الدكتور محمد عزيز الموسوي
2-الأستاذ الدكتور مساعد لفتة ألبدري
أعضاء المجلس العلمي
|
جهة العمل |
اللقب العلمي |
الاسم الثلاثي |
ت |
|
المجلس العراقي للاختصاصات الطبية |
أستاذ |
الدكتور ناصر عيدان ناصر |
|
|
ممثل كلية الطب / بغداد |
أستاذ مساعد |
الدكتور عزام محسن عباس |
|
|
ممثل وزارة الصحة |
استشاري |
الدكتور محمد ضياء احمد |
|
|
ممثل كلية الطب/ جامعة النهرين |
أستاذ مساعد |
الدكتور جعفر محمد كاظم |
|
|
ممثل كلية الطب/ الجامعة المستنصرية |
أستاذ |
الدكتور إيهاب طه ياسين |
|
|
ممثل كلية الطب/ جامعة بابل |
أستاذ |
الدكتور صفاء صاحب ناجي |
|
|
ممثل كلية الطب/ جامعة الكوفة |
أستاذ |
الدكتور احمد عذاب معيان |
|
|
ممثل كلية الطب/ جامعة القادسية |
أستاذ |
الدكتور قاسم ريسان دخيل |
|
|
ممثل كلية الطب/ جامعة البصرة |
أستاذ |
الدكتور احمد محمد مهودر |
|
|
ممثل كلية الطب/ جامعة السليمانية |
أستاذ مساعد |
الدكتور مؤيد إسماعيل عزيز |
|
|
ممثل كلية الطب/ جامعة أربيل |
أستاذ مساعد |
الدكتور ميسر عبد الرحمن ياسين |
|
|
ممثل كلية الطب/ جامعة الموصل |
أستاذ |
الدكتور علي عبد المطلب محمد |
|
|
ممثل كلية الطب/ جامعة كربلاء |
استشاري |
الدكتور أنور صادق جعفر |
|
هيكلية المجلس العلمي لجراحة الأنف والإذن والحنجرة للعام الدراسي 2020 - 2021
|
ت |
المركز التدريبي |
عدد الطلاب |
مسؤول المركز |
المشرفون |
المدربون |
|
|---|---|---|---|---|---|---|
|
|
م . الشهيد غازي الحرير للجراحات التخصصية |
14 |
ا. م. د عزام محسن عباس |
1- ا. م. د. عزام محسن عباس 2- ا. م. د . احمد محي رشيد 3- الاستشاري د. هاني موسى بدر 4- الاستشاري د. ثامر محسن عباس |
5- الاستشاري د. محمد ضياء احمد 6- الاستشاري د . رغيد تركي متعب 7- الاستشاري د. . ليث علي محمود |
لا يوجد |
|
|
م.الإمامين الكاظمين (ع) |
16 |
ا. م. د جعفر محمد كاظم |
1- ا.د ناصر عيدان ناصر 2- ا. م. د جعفر محمد كاظم 3- الاستشاري د. عادل نعيم رزوقي 4- الاستشاري فردوس فاضل عبد الرضا |
5- الاختصاصي د.حسام طالب داخل/ مدرب |
1 |
|
|
م. اليرموك التعليمي
|
16 |
ا. د إيهاب طه ياسين |
1- ا. د إيهاب طه ياسين 2- ا.د عمار هادي خماس 3- ا.م.د محمد رديف داود 4 - ا.م.د. فالح مهدي كاظم العنبكي |
5- الاستشاري د. بهاء محسن عباس 6- الاستشاري د. علاء مطشر طالب 7- الاستشاري د. ياسين أديب سكران 8- الاستشاري د. محمد حسن سعيد |
لا يوجد |
|
|
م. بابل التعليمي |
5 |
ا. د صفاء صاحب ناجي |
1- ا. د صفاء صاحب ناجي 2- ا. م د سعد عبد الرحيم حسين |
3- ا. م د ميثم لفتة كريم 4- الاستشاري د. صفاء نوري محمد |
لا يوجد |
|
|
م. الكوفة التعليمي |
8 |
ا. د احمد عذاب معيان |
1- ا. د احمد عذاب معيان 2-ا. د ياسر لفتة حسون حمزة 3- ا. م. د فراس موفق حسن |
لا يوجد |
|
|
|
م. الديوانية التعليمي |
5 |
ا. د قاسم ريسان دخيل |
1- ا. د قاسم ريسان دخيل 2- ا. د.راهي كلف مهدي |
3- الاستشاري د إياد احمد شهاب 4- الاستشاري د رائد يعقوب يوسف |
لا يوجد |
|
|
م . البصرة التعليمي |
6 |
ا. د احمد محمد مهودر العباسي |
1- ا. د احمد محمد العباسي 2- ا. د عصام محمد عبد المحسن 3- الاختصاصي د. علي عبد الوهاب ادريس/ مدرب |
1 |
|
|
|
م . السليمانية التعليمي |
12 |
ا . م. د . مؤيد إسماعيل عزيز |
1- ا . م. د . مؤيد إسماعيل عزيز 2- ا . م. د. هيوا اسعد عبد الكريم |
3- الاستشاري د. عقيل عبد الرزاق خضير
|
لا يوجد |
|
|
م . أربيل التعليمي |
14 |
ا. د .ميسر عبد الرحمن ياسين |
1- ا .د. ميسر عبد الرحمن ياسين 2- ا.د. سعيد مصطفى سعيد |
3- ا.م.د. أرسلان عولا مصطفى
|
لا يوجد |
|
|
م. الموصل التعليمي |
9 |
ا. د.علي عبد المطلب محمد |
1- ا. د.علي عبد المطلب محمد 2- ا. د.باسل محمد نذير سعيد 3- ا. م.د.هيثم عبد الملك
|
4- ألاستشاري د. رغدان محمد داود 5- ألاستشاري د. مروان فيصل برع |
لا يوجد |
|
|
م. كربلاء التعليمي
|
لا يوجد |
ألاستشاري د. أنور صادق جعفر |
ألاستشاري ناظم عمران كاظم ألاستشاري د. أنور صادق جعفر |
لا يوجد |
|
العدد الكلي للأساتذة + المشرفين+ المدربين للمجلس العلمي لجراحة الأنف و الإذن والحنجرة =48
العدد الكلي للطلبة للمجلس العلمي لجراحة الأنف و الإذن والحنجرة = 106
العدد الكلي للمراكز التدريبية للمجلس العلمي لجراحة الأنف و الإذن والحنجرة= 11
The Otolaryngology curriculum provides the approved framework for the training of doctors to the level of independent specialist practice in Otolaryngology surgery, addressing the requirements of patients, the population, and the strategic health services.
Mission
The Otolaryngology Council of the Iraqi Board for Medical Specializations through its (5 Years) program aiming at certifying high quality, safe ENT specialists who can work in Iraq and competing with their counterpart outside by complying with regional and global standard.
The purpose of the curriculum is to produce, at certification, specialist Otolaryngology surgeons with the generic and specialty-specific professional capabilities needed to manage patients presenting with the full range of acute conditions and general elective conditions as well as to develop a special interest within Otolaryngology.
This section of the curriculum defines the scope of practice of Otolaryngology, what has to be learned, the levels of performance expected to complete training, how the curriculum is delivered and how it is assessed.
Patient safety and competent practice are both essential and the curriculum has been designed so that the learning experience itself should not negatively affect patient safety. Patient safety is the first priority of training demonstrated through safety-critical content, expected levels of performance, critical progression points, required breadth of experience, and levels of trainer supervision needed for safe and professional practice. Upon satisfactory completion of training programs, trainees are expected to be able to work safely and competently in the defined area of practice and to be able to manage or mitigate relevant risks effectively. A feature of the curriculum is that it promotes and encourages excellence through the setting of high-level outcomes, supervision levels for excellence, and tailored assessment and feedback, allowing trainees to progress at their own rate.
Training is divided into two phases, the first one that lasts for 1 year divided between general surgery and three other related specialties.
The second phase for the other four years of training should cover the major areas in otolaryngology.
The curriculum ensures that trainees at certification, have both a special interest skill and good general emergency and elective skills. Six special interest areas are offered:
The Otolaryngology curriculum will produce a workforce fit for the needs of patients, producing doctors who are more patient-focused, more general and who have more flexibility in their career structure. All the shared Capabilities in Practice are transferable to other surgical specialties and some may be transferable to non-surgical specialties. In addition, core knowledge and skills gained in any surgical specialty training programme are transferable for entry into Otolaryngology. Trainees who choose to move to or from a different specialty training programme having previously gained skills transferable to Otolaryngology, therefore, may be able to have a shorter than usual training pathway in their new training programme. While most of the specialty syllabus is not transferable because the knowledge and detailed technical skills are specific to Otolaryngology, some limited areas of the syllabus may be transferable e.g. Thyroid and Parathyroid surgery could be transferred to the Endocrine Surgery special interest within General Surgery. This flexible approach, with acquisition of transferable capabilities, allows surgical training to adapt to current and future patient and workforce needs and change in the requirements of surgery with the advent of new treatments and technologies.
Trainees enter Otolaryngology training via a national selection process, having successfully completed the curriculum for 1 year ENT Senior clinical fellow (SHO) training and been successful at ENT written exam with minimum 70% score.
Duration of training in otolaryngology specialty is five years divided as follows:
Phase I
One year divided as follows:
6 months general surgery
2 months of plastic surgery
2 months neurosurgery
2 months maxillofacial surgery
Phase II
Four years otolaryngology
In phase one the trainee should follow the core surgical training curriculum, and at end of this phase should pass a primary written examination in principles and basic knowledge of general surgery and basic science in otolaryngology.
During phase 2, trainees must gain the knowledge and clinical skills in general Otolaryngology to the level of independent practice expected at certification.
At certification, trainees must be able to manage a wide range of general Otolaryngology elective and emergency procedures in both children and adults which should be documented by logbook Yearly.
A thesis should be achieved in the Otolaryngology specialty and should be accepted by the committee at the end of 3rd year.
A mid examination should be passed at the end of the 4th year.
On successful completion of final written and clinical examination in general otolaryngology at the end of the 5th year, trainees become eligible for certification and for recommendation to enter the specialist register.
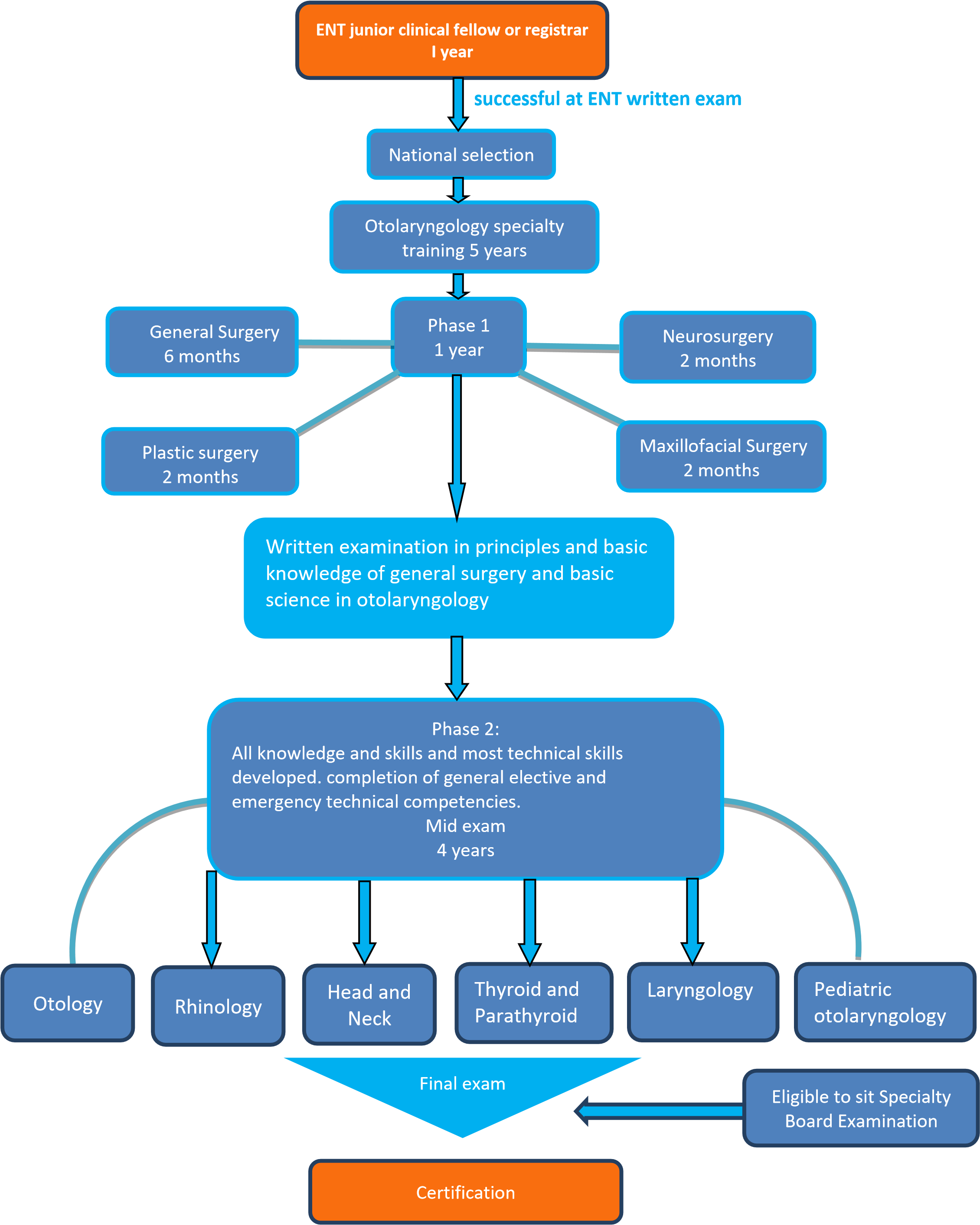
Figure 1: Otolaryngology training pathway.
This section covers the expected learning outcomes, learning methods, breadth of experience and levels of performance at critical progression points in the training Programme and the levels of performance expected of those completing training.
The practice of Otolaryngology requires the generic and specialty knowledge, clinical and technical skills and behaviors to manage patients presenting with a wide range of ear, nose, throat and neck disorders. It involves development of competence in diagnostic reasoning, managing uncertainty, dealing with co-morbidities, and recognizing when another specialty opinion or care is required.
Training is designed to produce a person capable of safely and effectively performing the role of a first day specialist surgeon. The role of a specialist surgeon can be thought of as a sum of all the various tasks which need to be performed through a working week. These tasks are the high-level outcomes of the curriculum and grouping these together describe the role of a specialist surgeon. To perform a high-level clinical task as a specialist surgeon requires trainees to be able to integrate areas of learning from all parts of the syllabus, including knowledge, clinical skills, professional skills and technical skills. In addition, a surgeon will need to have acquired the generic skills, behaviors and values shared by all doctors in order to perform this task safely and well. A capability is a set of skills that can be developed through training from novice to expert and, therefore, these high-level clinical outcomes are known as Capabilities in Practice.
There are five Capabilities in Practice which are shared between all surgical specialties:
The curriculum requires trainees to accrue a rich experience that promotes deep learning of knowledge, clinical skills, technical skills, professional behavior, leadership and all other generic professional skills that are considered necessary to ensure patient safety throughout the training process and specifically at the end of training. The scope of practice of a day-one consultant in Otolaryngology is described in the syllabus. In addition, there are certain skills and conditions within the syllabus that are of such central and fundamental importance to the safe practice of Otolaryngology that they are highlighted as critical conditions and index procedures.
From the syllabus, a list of critical conditions has been identified which are of significant importance for patient safety and demonstration of a safe breadth of practice. Across surgery, these are defined as any condition where a misdiagnosis could be associated with devastating consequences for life or limb. These critical conditions are assessed individually by means of the Case Based which include an assessment of clinical judgement and decision-making. They provide formative feedback to the trainee and feed into the summative assessment of the Assigned Educational Supervisor.
The curriculum is used to help design training programmes locally that ensure all trainees can develop the necessary skills and knowledge in a variety of settings and situations. The curriculum is designed to ensure it can be applied in a flexible manner, meeting service needs as well as supporting each trainee’s own tailored learning and development plan. This stipulates that all training must comply with the following standards:
Theme 1: learning environment and culture
S1.1 The learning environment is safe for patients and supportive for learners and educators. The culture is caring, compassionate and provides a good standard of care and experience for patients, carers and families.
S1.2 The learning environment and organisational culture value and support education and training, so that learners are able to demonstrate what is expected in Good Medical Practice and to achieve the learning outcomes required by their curriculum.
Theme 2: educational governance and leadership
S2.1 The educational governance system continuously improves the quality and outcomes of education and training by measuring performance against the standards, demonstrating accountability and responding when standards are not being met.
S2.2 The educational and clinical governance systems are integrated, allowing organisations to address concerns about patient safety, the standard of care, and the standard of education and training.
S2.3 The educational governance system makes sure that education and training is fair and is based on the principles of equality and diversity.
Theme 3: supporting learners
S3.1 Learners receive educational and pastoral support to be able to demonstrate what is expected in Good Medical Practice, and to achieve the learning outcomes required by their curriculum.
Theme 4: supporting educators
S4.1 Educators are selected, inducted, trained, and appraised to reflect their education and training responsibilities.
S4.2 Educators receive the support, resources and time to meet their education and training responsibilities.
A variety of educational approaches are used by education providers in order to help trainees develop the knowledge, clinical and technical skills, professional judgement, values and behaviors required by the curriculum. These educational approaches divide into three areas:
4.2.1 Self-directed learning
The curriculum is trainee-led and self-directed learning is encouraged. Trainees are expected to take a proactive approach to learning and development and towards working as a member of a multi-professional team. Trainees are encouraged to establish study groups, journal clubs and conduct peer reviews. They should take the opportunity of learning with peers at a local level through postgraduate teaching and discussion sessions, and nationally with examination preparation courses. Trainees are expected to undertake personal study in addition to attending formal and informal teaching. This includes using study materials and publications and reflective practice. Trainees are expected to use the developmental feedback they get from their trainers in learning agreement meetings and from assessments to focus further research and practice.
Reflective practice is an important part of self-directed learning and of continuing professional development. It is an educational exercise that enables trainees to explore, with rigour, the complexities and underpinning elements of their actions in order to refine and improve them. Reflection in the oral form is very much an activity that surgeons engage in and find useful and developmental. Writing reflectively adds more to the oral process by deepening the understanding of practice. Written reflection offers different benefits to oral reflection which include: a record for later review, a reference point to demonstrate development and a starting point for shared discussion. Whatever the modality of reflection, it is important that it takes place and that there is a record of it having taken place, whether or not the specific subject or content of the reflection is recorded.
4.2.2 Learning from clinical practice
Surgical learning is largely experiential in nature with any interaction in the workplace having the potential to become a learning episode. The workplace provides learning opportunities on a daily basis for surgical trainees, based on what they see and what they do. Trainees are placed in clinical placements, which provide teaching and learning opportunities. The placements must be in units that are able to provide sufficient clinical resources and have sufficient trainer capacity.
While in the workplace, trainees are involved in supervised clinical practice, primarily in a hospital environment in wards, clinics or theatre. There are strong links to practitioners working in primary care and training environments may include private settings and, where available for training, a variety of community settings where the necessary facilities and governance arrangements are in place. The trainee role in these contexts determines the nature of the learning experience. Learning begins with observation of a trainer (not necessarily a doctor) and progresses to assisting a trainer; the trainer assisting/supervising the trainee and then the trainee managing a case independently but with access to their supervisor. The level of supervision changes in line with the trainee’s progression through the phases of the curriculum. As training progresses, trainees should have the opportunity for increased autonomy, consistent with safe and effective care for the patient. Typically, there should be a gradual reduction in the level of supervision required and an increase in the complexity of cases managed until the level of competence for independent practice is acquired.
4.2.3 Learning from formal situations
Learning from clinical practice is supplemented by an educational programme of courses and teaching sessions arranged at local, regional and national levels.
Supervision is fundamental in the delivery of safe and effective training. It takes advantage of the experience, knowledge and skills of expert clinicians and ensures interaction between an experienced clinician and a trainee. The ultimate responsibility for the quality of patient care and the quality of training lies with the supervisor. Supervision is designed to ensure the safety of the patient by encouraging safe and effective practice and professional conduct. A number of people from a range of professional groups are involved in teaching and training with subject areas of the curriculum being taught by staff with relevant specialist expertise and knowledge.
Those involved in the supervision of trainees must have the relevant qualifications, experience, and training to undertake the role. Specialist skills and knowledge are usually taught by consultants and senior trainees whereas the more generic aspects of practice can also be taught by the wider multidisciplinary team MDT).
Effective feedback is known to enhance learning, and combining self-reflection with feedback promotes deeper learning. Trainees are encouraged to seek feedback on all they do, either informally, through verbal feedback at the end of a learning event.
All trainees are required to satisfy the learning outcomes: Capabilities in research and scholarship. Trainees are encouraged to participate in clinical research and collaborative trials to achieve these outcomes, as well as in journal clubs, literature review and systematic review and to make a major contribution to the publication of novel findings in peer reviewed journals. An understanding of the principles of research, its interpretation and safe implementation of evidenced based new methods, processes and techniques is essential for the modern, progressive practice of surgery and in the interests of patients and the service.
The specialty elements of the early years will all be assessed primarily in the workplace and then scrutinised in the Annual Review of Competency Progression. Specific evidence includes:
4.6.1 Doctor AssessmentForm (competencies feedback form)
A. ENT Senior clinical fellow (registrar) (1 year)
B. Core trainee in otolaryngology specialty (5 years)